TMS For Stroke: A New Era in Stroke Rehabilitation
Stroke is a life-altering event that affects millions of people each year. Survivors often face significant physical, emotional, and cognitive challenges, making rehabilitation a crucial part of recovery. Traditional therapies — such as physical therapy, occupational therapy, and speech-language therapy — have long been the foundation of stroke rehabilitation. However, recent advancements in neuroscience have introduced new tools that can enhance recovery. One of the most promising of these tools is Transcranial Magnetic Stimulation (TMS).
This blog explores how TMS For Stroke can support and accelerate recovery, the science behind it, its clinical benefits, and what patients and caregivers need to know.
What Is TMS?
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain. TMS is widely known for treating depression, but its potential in stroke rehabilitation is becoming increasingly recognized in both clinical settings and research communities.
The procedure involves placing a magnetic coil on the scalp near the targeted area of the brain. This coil generates brief magnetic pulses that stimulate brain activity in regions responsible for motor control, speech, mood, and cognition.
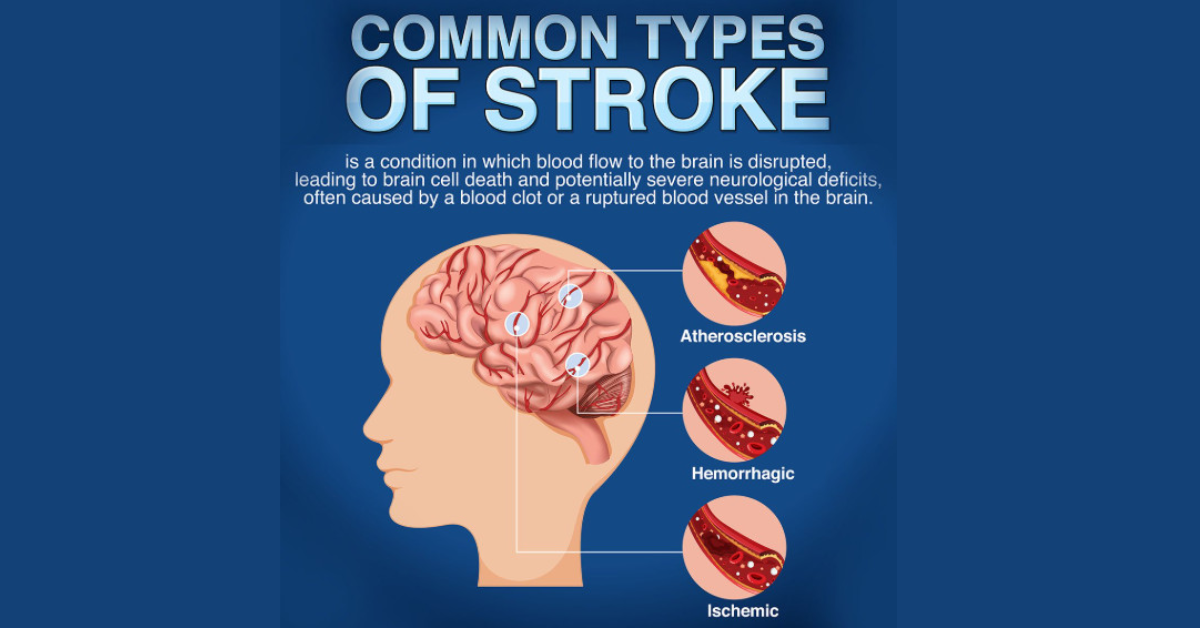
Understanding the Impact of Stroke
Stroke occurs when blood flow to a part of the brain is interrupted, either due to a clot (ischemic stroke) or a bleed (hemorrhagic stroke). The lack of oxygen and nutrients can lead to brain cell death and result in:
-
Partial paralysis or muscle weakness
-
Impaired speech and language (aphasia)
-
Difficulty with walking and balance
-
Cognitive challenges such as memory and concentration
-
Emotional and psychological effects, including depression and anxiety
Traditional stroke rehabilitation focuses on helping patients relearn lost skills through repetitive exercises and therapeutic interventions. While effective, recovery can be slow and incomplete for many. This has led researchers to explore ways to enhance brain recovery, including through neuromodulation techniques like TMS.
How TMS Helps Stroke Patients
TMS supports stroke recovery by directly influencing neural circuits involved in movement, cognition, and emotion. Here’s how it works:
1. Stimulating Neuroplasticity
After a stroke, the brain can reorganize itself by forming new neural connections — a process known as neuroplasticity. TMS enhances neuroplasticity by stimulating underactive or damaged areas of the brain, helping to “rewire” neural pathways and improve function.
2. Balancing Brain Hemispheres
In many stroke cases, one hemisphere of the brain (typically the damaged side) becomes less active, while the opposite hemisphere becomes overactive. This imbalance can hinder recovery. TMS can either excite the affected hemisphere or inhibit the overactive hemisphere, restoring a more functional balance.
3. Improving Motor Function
Motor impairment is a common consequence of stroke, particularly in the hands, arms, and legs. By targeting the motor cortex, TMS has shown promising results in improving strength, coordination, and voluntary movement.
4. Enhancing Speech and Language
Patients with aphasia — difficulty in speaking or understanding speech — can benefit from TMS. Stimulating language-related areas of the brain, especially in the left hemisphere, has been shown to improve speech production and comprehension in some stroke survivors.
5. Alleviating Post-Stroke Depression
Depression is common after a stroke and can reduce motivation and participation in therapy. TMS is FDA-approved for treatment-resistant depression and can help improve mood, energy, and cognitive engagement in stroke survivors.
Clinical Evidence Supporting TMS for Stroke
Clinical trials and peer-reviewed studies increasingly support the use of TMS in stroke rehabilitation. For example:
-
A 2020 study published in Stroke demonstrated significant improvement in upper limb motor function in stroke patients treated with repetitive TMS (rTMS).
-
Research from Harvard Medical School highlighted the benefits of TMS in restoring interhemispheric balance, which is key to improving motor outcomes.
-
International studies on language recovery have shown that TMS can facilitate naming and speech fluency in patients with post-stroke aphasia.
While TMS is not yet a universal standard in stroke rehabilitation, its clinical backing is growing, and more medical centers are incorporating it into treatment plans.
What to Expect During a TMS Session
Evaluation and Planning
Before starting treatment, a specialist conducts a thorough assessment that includes medical history, imaging (such as MRI), and cognitive and motor function evaluations. This helps identify the areas of the brain to be targeted.
The Treatment Process
-
Sessions typically last 20 to 40 minutes.
-
Patients remain fully awake and seated during treatment.
-
A magnetic coil is positioned on the scalp, and pulses are delivered to the target area.
-
Most patients describe the sensation as a light tapping on the scalp.
TMS treatments are usually conducted daily, five times a week, for four to six weeks. The number of sessions depends on the individual’s condition and response to therapy.
Post-Treatment Monitoring
Throughout the treatment course, progress is monitored regularly. TMS is often combined with physical, occupational, or speech therapy for a comprehensive rehabilitation approach.
Is TMS Safe for Stroke Patients?
TMS is generally considered safe and well-tolerated when administered by trained professionals.
Common Side Effects:
-
Mild headache or scalp discomfort
-
Temporary facial muscle twitching during treatment
-
Tingling sensations in the scalp
Rare Side Effects:
-
Seizures (extremely rare, especially when safety guidelines are followed)
-
Temporary hearing discomfort (protective earplugs are typically used)
TMS is non-invasive and does not require anesthesia or recovery time. Most patients can return to their daily activities immediately after each session.
Who Is a Good Candidate for TMS After Stroke?
TMS may be suitable for stroke survivors who:
-
Have persistent motor or cognitive deficits despite conventional therapy
-
Experience post-stroke depression or apathy
-
Are medically stable and cleared by their physician
-
Are in either the subacute (1–6 months) or chronic (>6 months) phase of stroke recovery
TMS is not recommended for individuals with a history of seizures, metal implants in the skull, or certain neurological conditions without further medical evaluation.
Integrating TMS With Traditional Therapy
TMS is most effective when used as part of a comprehensive stroke rehabilitation program. It complements:
-
Physical therapy, by enhancing motor learning and coordination
-
Occupational therapy, by improving functional task performance
-
Speech therapy, by facilitating language and communication recovery
-
Psychological counseling, by supporting emotional and cognitive health
This integrative approach maximizes brain recovery and leads to better long-term outcomes.
The Future of TMS in Stroke Rehabilitation
As the technology continues to advance, the role of TMS in stroke recovery is expanding. Future developments may include:
-
Personalized TMS protocols, based on individual brain imaging
-
Portable and home-based TMS systems
-
Combination with neurofeedback, robotics, or virtual reality therapies
-
Use in acute stroke settings, potentially reducing long-term disability
Continued research and clinical trials are likely to establish TMS as a mainstream option for stroke rehabilitation.
Frequently Asked Questions (FAQs)
1. Is TMS approved for stroke recovery?
TMS is FDA-approved for depression but used off-label for stroke rehabilitation. However, growing evidence supports its effectiveness, and it is used in many advanced rehabilitation centers.
2. How soon after a stroke can TMS be started?
TMS can be initiated a few weeks post-stroke in some cases, but most protocols begin during the subacute or chronic recovery phase. Your physician will determine the best time to start.
3. Does TMS replace physical therapy?
No. TMS is designed to complement, not replace, conventional rehabilitation therapies. It is most effective when integrated into a broader treatment plan.
4. Are the results of TMS permanent?
TMS promotes lasting brain changes, but some patients may require booster sessions. Ongoing rehabilitation and healthy lifestyle choices also support long-term benefits.
5. Can elderly patients benefit from TMS?
Yes. Age is not a strict limitation. Many older adults experience improvements with TMS, especially when customized to their needs and health status.
Conclusion
TMS for stroke is an exciting advancement in the field of neurorehabilitation. By enhancing brain plasticity and supporting traditional therapy methods, TMS offers stroke survivors new hope for regaining mobility, speech, and cognitive function.
While it is not a cure-all, TMS represents a significant step forward in helping individuals recover more fully and live more independently after a stroke. If you or a loved one is navigating the journey of stroke recovery, TMS may be worth exploring as part of a comprehensive treatment plan guided by experienced professionals.